Healthcare has been through a paradox of rising costs and unsteady outcomes, which are just among the problems that the system faces. Patients repeatedly undergo fragmented care, find themselves in hospital admission situations that could have been prevented, and have complications that could have been avoided, situations that clearly indicate the need for thorough systemic reform.
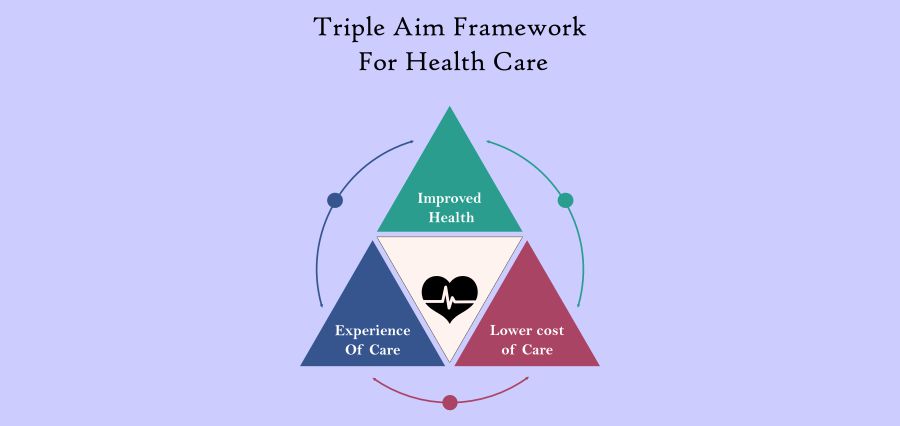
To tackle these problems, the triple aim sets three interconnected objectives that work hand in hand, striving for healthcare systems to give better value without making compromises. These objectives—betterment of the health care experience of patients, elevating population health, and lowering the per capita healthcare costs—are mutually reinforcing in design. The potency of this model rests on the success being dependent on the accomplishment of all three aims at the same time, rather than on just one, giving priority.
Take, for example, the objective of patient satisfaction; if community health risks had not been addressed, surely this goal would have done very little in terms of reducing costs. Similarly, if costs are reduced by eliminating critical services, then this will put the outcomes at risk. The triple aim is a forceful advocate of balance, which is what renders it one of the most revolutionary benchmarks of healthcare reform currently existing.
The Triple Aim as the Patient-Cantered Care Alien
People are at the centre of the triple aim, in contrast to what many might think it to be. The first pillar of the triple aim points out the relevance of patient-centred care, which is the most important factor in the healthcare experience of patients at each stage of their journey. Besides medical treatment, the way patients are emotionally, mentally, and socially handled by providers is also counted in this. A positive, compassionate experience creates in patients a feeling of trust, adherence, and eventually better health outcomes.
Today’s patients desire more than just getting rid of their illnesses. They want the truth communicated openly, shorter waiting times, digital access to their health data, and more comprehensive approaches that consider their uniqueness. Healthcare organizations that fall under the triple aim healthcare model mainly direct their resources to empathy-centric innovations such as telemedicine, community health programs, and personalized treatment plans. These bring about patient satisfaction largely while making sure that the treatment that patients receive is smooth across different healthcare providers.
Population Health Strengthening
The triple aim’s population health is the other major and an equally necessary aspect. Compared to the conventional framework that focuses mainly on the treatment of diseases, population health puts an emphasis on prevention, lifestyle changes, and public health measures that aim at community-wide risk reduction. The social determinants of health, such as education, housing, and access to food, have a huge impact on chronic conditions like diabetes, high blood pressure, and obesity.
Healthcare providers using the triple aim’s philosophy thus penetrate beyond clinical walls to grasp the broader picture. A case in point is collaborating with community organizations that work on food insecurity or physical activity, health issues that might be a cause of chronic diseases over time, hence the rate of chronic illnesses can be reduced. With screening programs, early interventions, and outreach activities directed at the at-risk groups, the problems are more manageable before they escalate.
Lowering costs without compromising quality
The third aspect of triple aim is often the root of most talk: how can transformation of the system use drop expenses while augmenting outcomes? The solution could be found not in reducing services but rather in cutting inefficiencies and focusing on value-driven care.
Avoidable hospital readmissions, visits to emergency rooms that are unnecessary, and repeated tests are just a few examples of waste that can be very expensive. Healthcare organizations can cut down on unnecessary costs while making sure that more resources are available for those interventions that matter by changing the way healthcare is delivered.
Providers who are implementing triple aim healthcare strategies have, in many cases, gone for payment models that remunerate value instead of volume. Such an approach promotes the idea of keeping patients well, instead of merely treating them for their diseases, since value is the focus. Coordinated care, digital monitoring devices, and tighter partnerships between providers help to remove the overlap and lighten the patient’s road, which saves not only money but also his time and reduces his worries as far as he is concerned.
The Interconnected Power of the Triple Aim
One of the main reasons why the triple aim works so well is that the different goals largely support each other. To be more specific, better patient experiences generally result in higher adherence, and improved adherence eventually boosts the overall health of the community. In the end, a healthier population means fewer hospitals and insurance companies’ workloads, thus lower expenses. This cyclical pattern of improvement shows the reason why the triple aim is considered by many policy-makers, insurers, and providers as the gold standard for reform.
Nevertheless, it is far from easy to reach this equilibrium. Collaboration of approaches from a wide array of sectors, such as clinics, hospitals, schools, government organizations, and even businesses, is required. Along with this, it demands new performance measures. Considering only the number of cases handled is no longer sufficient; organizations at this point must focus on outcomes that mirror the quality of life, equity, and access to care.
Future of The Triple Aim Model
Over the next few years, the triple aim healthcare model will keep having a significant impact on policymaking and practical applications. The crisis brought on by the COVID-19 pandemic highlighted strengths needed in healthcare systems and pointed out the big flaws. Consequently, entities are increasingly moving to embrace the triple aim for creating new systems that are not only stronger but also more agile and can easily cope with any future crisis.
Innovations in technology will be one of the highlights of this era. Digital health tools, AI, and remote monitoring have broadened the possibilities to engage patients beyond the conventional settings. Moreover, there is an increasing understanding that the health care sector alone cannot manage the problem. The triple aim can only labour if levers such as addressing the social determinants of health, widening the preventive care sphere, and focusing on compassion are put to work.
The triple aim is not merely a strategic framework; it is a concept that makes one think about the entirety of the healthcare system’s influence on human lives. Through patient-centred experiences, community health, and cost efficiency, all being dealt with simultaneously, health care providers can establish sustainable systems that promote public health. Patients will enjoy better care. For communities, it means healthier and more equitable outcomes. And for healthcare systems, it is a map that guides the value delivery without sacrifice.
In the time that demands are increasing and resources are dwindling, the triple aim’s theme of equilibrium and progress acts as a feasible route to move forward. The triple aim’s message is both totally revolutionary and very simple: it is not only possible to improve health for people and communities but also necessary.